Reflective practice in context: Health
Reflective practice in healthcare starts from your time as a student and continues throughout your professional career. It’s embedded in health sciences and allied health courses, from medicine, paramedicine and nursing to psychology, physiotherapy and nutrition science. It’s an ongoing, career-long practice, so it’s a good idea to build up your reflective skills as early as possible. Critical reflection is a useful learning tool. It requires you to analyse a feeling or experience and learn from it, so you know what to do better next time.
As a health student or professional, you might reflect on challenges or things that go wrong, like:
- an incorrect diagnosis or clinical decision
- an uncomfortable interaction with a patient or poor rapport in general
- personal bias or a cultural sensitivity misstep
- a breakdown in communication
- staff burnout
- an ethical dilemma or boundary issue.
There are also plenty of positive things that you might reflect on to ensure your practice remains at a high standard, such as:
- beneficial classes or professional development sessions you’ve attended
- positive feedback from a patient or client
- a successful new approach you have tried with a patient
- implementing self-care strategies
- effective collaborative experiences
- a well-managed emergency procedure.
These different types of reflections might require a formal, written document or just an informal chat with a colleague or clinical placement supervisor. Reflective practice is done both independently and collaboratively, depending on the situation and the person’s needs and preferences.
Check out the pages in this chapter on reflective thinking and practice and reflective writing, if you would like to get a more general background.
Why is reflective practice important in the healthcare industry?
Everyone benefits from a culture of valuing and participating in reflective practice: the health professional, their colleagues and patients, and the healthcare system as a whole.
Here are just some of the benefits:
To learn more about reflective practice in health and its benefits, watch this helpful video by the Clinical Excellence Commission:
Writing a reflective journal entry
Medicine, nursing, allied health and health science courses generally have a professional placement component. During your placement, you will be required to demonstrate your progress by reflecting on your experiences and what you have learnt. This is also an opportunity for your supervisor and educators to assess your critical reflection competency. A common form of assessment is a reflective journal, which you write in regularly and discuss with your mentor, supervisor, trainer, or teacher.
The Gibbs’ Reflective Cycle is a model that is often used to structure reflective writing tasks. It was developed by Graham Gibbs in his 1988 book ‘Learning by Doing’ and has proved to be popular in many professional fields, including those in the healthcare sector.
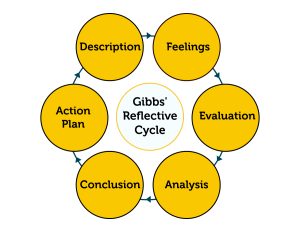
The information below explains each step of the model and shows its application. You can expand each section, or access the transcript, to read an example of a nursing student’s reflective journal entry.
Description
This is where you describe what has happened. You need to set the context for your reflection, but don’t start interpreting it yet. Include the details and facts of the situation or experience you are reflecting on.
Feelings
This is where you include your thoughts and feelings from your own perspective. Write about how you felt at the time of the event and afterwards.
Evaluation
This is where you write about what was good and what was challenging about the situation. What are the things that worked and what didn’t? Comment on any strengths and weaknesses you noticed in your own skills or knowledge and explain the ways in which the experience was important to you and others.
Analysis
This is where you discuss the things which contributed to the positive and negative aspects of the experience and how things could have been different. It’s usually the longest part of the model. You should explain what you have learnt from the situation and your reflection on it. You might also include references to theories you’ve studied in class or articles you’ve read for your course.
Conclusion
This is where you summarise the insights you’ve gained and explain how the experience has contributed to your professional growth. Comment on what you’re pleased with and what you need to do better next time.
Action Plan
This is where you write about the steps you’re going to take based on your reflection, and how you will apply your learning to future situations. Comment on the changes or improvements you will make and how.
Reflect
Consistently working through a reflective process, even if it’s just chatting to friends or thinking things over while you have lunch, will help develop your skills. Try introducing reflection into your daily routine – it’s as easy as considering your answers to some reflective prompts. Here are some to help you get started:
- Do you find it difficult to get along with or relate to any patients? Why do you think this is? How does it make you feel?
- What’s something (big or small) that has made you feel capable and proud this week? What led to this experience?
- What’s something you’ve learnt lately that has surprised or interested you? What will you do with this knowledge going forward?
- Have you encountered any misunderstandings this week? What caused them? Consider this from the perspective of everyone involved.
- Is there anything you’d like to change about the health-care profession you’re in? How would you change it?
- Have you felt anxious or upset while studying or working in your healthcare field? What do you think contributed to those feelings?
Another way to reflect, is to think back over your day and seek out the learning moments. Driscoll’s reflective model is easy to follow when you’re reflecting informally but still want a bit of structure.
- ‘What?’ – What happened?
- ‘So what?’ – Why does it matter? Consider why the experience is important.
- ‘Now what?’ -What have you learnt and what will you do? Plan your next steps based on what you’ve learnt from the experience.
Example:
What? I did my first independent consultation today. I created a personalised meal plan with the patient, but she seemed frustrated and resistant to my recommendations. She told me that she was tired of health professionals ‘bossing her around’, so I changed my approach, and at the end of the session she said she was pleased with how our consultation went overall.
So what? I think this was okay for my first consultation, but it might not have been if I hadn’t noticed the patient’s demeanor. In the past, patients have responded well to my naturally authoritative tone, but my patient today clearly didn’t feel comfortable with this approach. When I asked her to give me more feedback on the plan and made changes based on her comments, she became much more receptive. This experience has made me realise that there might be less outspoken patients who feel pushed around by medical professionals and my communication style may contribute to this.
Now what? I’ve learnt that one communication style will not suit all patients and that I should seek patients’ input more. In future, I’ll consider the patient’s communication style at the beginning of a consultation and adapt my own to suit the dynamic they set. I’ll encourage them to collaborate on the plan, and I’ll also ask patients whether the plan aligns with their preferences and lifestyle.
As you have learnt, reflective practice contributes to continuous improvement and creating the best conditions for you, your colleagues, and your patients. You will engage in reflective thinking, writing, and discussions during your studies, your professional placement, and in your future role as a health professional – so it’s important to know how to do it well and get the most out of it. The ability to reflect on your experiential learning and improve your practice is not only essential in the healthcare sector – it’s a transferable skill that is highly valued across all industries. You can explore the other pages in this chapter to learn more about reflective practice in general and in other disciplines.
To learn more about reflective writing in nursing, check out the Learning Lab tutorial on writing a critical incident reflection.
Gibbs, G. (1988). Learning by doing: A guide to teaching and learning methods. Further Educational Unit, Oxford Polytechnic, Oxford.
Clinical Excellence Commission. (n.d) Reflective Practice. https://www.cec.health.nsw.gov.au/improve-quality/teamwork-culture-pcc/teamwork/reflective-practice
Clinical Excellence Commission. (2002) Reflective Practice workbook. https://www.cec.health.nsw.gov.au/__data/assets/pdf_file/0010/750529/reflective-practice-workbook.pdf
Clinical Excellence Commission. (2023) Reflective Practice. [YouTube video]. https://www.youtube.com/watch?v=pdlyKZhJbts&t=3s